Overview of Dyslipidemia
Dyslipidemia is a leading risk factor for cardiovascular diseases (CVDs). Therefore, PCPs must create an in-clinic workflow and clear approach for screening, risk evaluation, diagnosis, and treating dyslipidemia in their practices.
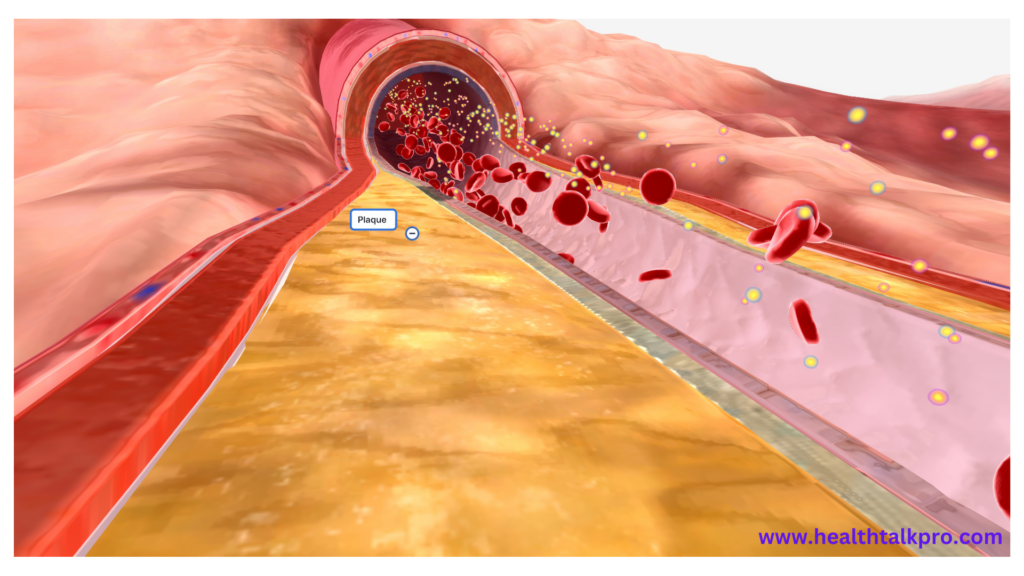
High levels of cholesterol can contribute to atherosclerosis, which reduces blood flow and increases the risk for a heart attack or stroke. High triglyceride levels may also result in yellow fat deposits on skin called xanthelasmas or around eyes, which impair vision, or lead to yellow fat accumulations known as xanthelasmas that form yellow spots on vision.
Causes
Lipids are taken up through the digestive process and transported throughout the body using lipoproteins for use as energy, steroid production, or bile acid formation. When levels become excessively high, however, they may increase cardiovascular disease risks such as coronary heart disease and stroke; high levels of LDL cholesterol or triglycerides may contribute to plaque formation within arterial walls, known as atherosclerosis; while increasing HDL cholesterol reduces this risk by flushing LDL from circulation more effectively.
Dyslipidemia can be caused by lifestyle factors like physical inactivity and eating too many saturated, trans, and monounsaturated fats or by other medical conditions that alter the amount of lipids in the blood, including diabetes mellitus, hypothyroidism, chronic kidney disease, and liver disease. Other potential contributors could include hereditary (familial) hypercholesterolemia as well as genetic abnormalities of lipid metabolism.
Elevated triglyceride levels may also be caused by certain medications used to treat HIV infection, including protease inhibitors and other protease inhibitors. Patients taking such drugs should monitor their triglyceride levels two or three months after beginning or switching therapies and annually thereafter; additionally, a low-fat diet and exercise, if not managed through medication alone, should also be recommended. In some instances, herbal supplements such as red yeast extract, garlic, policosanol, and niacin may help lower levels; these should only be taken under the medical advice of a healthcare provider.
Symptoms
Dyslipidemia symptoms depend on the nature and severity of abnormal lipid levels. High levels of cholesterol or triglycerides may lead to coronary heart disease by leading to plaque buildup in arteries; rupture of these plaques could result in a heart attack or stroke. High triglyceride levels can also damage livers and pancreas, while those suffering familial hypertriglyceridemia, where their triglyceride levels increase due to genetic mutation, may develop fatty deposits under their skin known as eruptive xanthomas.
Dyslipidemia is a serious health concern that increases your risk for cardiovascular diseases. Regular screening for dyslipidemia should include taking a lipid profile test that measures your LDL/HDL ratio as well as your triglyceride levels and other measures related to blood vessel health. Other tests measuring these functions are also helpful.
Diet and lifestyle modifications are key in treating dyslipidemia, particularly saturated and trans fat consumption, and lowering cholesterol levels. Consult your doctor regarding which diet choices would work best for you, while exercise, weight loss strategies, and stress management techniques may also be effective in lowering them. Talk to your physician if other medical conditions, such as diabetes or hypothyroidism, exist that require medication in addition to dyslipidemia treatment.
Treatment
Medication and dietary supplements available to lower cholesterol levels include bile acid sequestrants, HMG-CoA reductase inhibitors, and nicotinic acid; these may be combined for optimal results. In terms of diet changes that could help with dyslipidemia, they include avoiding foods with saturated and trans fats as well as increasing fiber consumption while cutting back on meats with high cholesterol content and cutting back on alcohol consumption.
Secondary dyslipidemia can be caused by lifestyle and medical factors that alter lipoprotein and lipid production and breakdown. Examples include physical inactivity, poor diet, obesity, diabetes, hypothyroidism, chronic kidney disease, liver disease, as well as certain drugs used to treat them. Treatment for secondary dyslipidemia typically centers on treating its source condition while attenuating any subsequent abnormalities to lipoprotein and lipid levels secondarily.
Screening for dyslipidemia is essential, particularly among individuals at increased risk, such as those with family histories of cardiovascular (CV) disease. Patients should have their fasting lipid profiles taken regularly depending on age and risk; adults should receive this screening every four to six years, while children and adolescents require screening every two to three years. Treatment goals include decreasing LDL cholesterol and triglycerides while raising HDL levels; additionally, it may address hypertension and diabetes risk factors as well.
Diagnosis
Dyslipidemia can be diagnosed by laboratory tests that measure total cholesterol, low-density lipoprotein (LDL) cholesterol, and triglyceride levels in the blood. Such measurements provide important clues as to an individual’s risk for cardiovascular disease; those with higher LDL levels or triglyceride counts tend to have increased chances of heart attack or stroke compared with their counterparts with normal levels.
Most people with high cholesterol don’t show symptoms; however, those with dyslipidemia may exhibit symptoms. These may include yellowish fat deposits forming plaques or nodules on hands, feet, or hands in general; a corneal arcus (a gray or white ring around the center of their eye’s cornea that indicates very high cholesterol levels); as well as other indicators like fatty tongues, swollen legs, or an increased heart rate as indicators.
Treating dyslipidemia requires treating its source, whether this means altering diet and physical activity levels, limiting alcohol consumption, or using medication such as statins (which work by inhibiting the 3-hydroxy-3methylglutaryl coenzyme A reductase enzyme). People diagnosed with clinical atherosclerotic cardiovascular disease (ASCVD) should receive high-intensity statins; those at risk should receive moderate-intensity statins; both types reduce LDL and triglycerides and raise HDL levels while raising HDL.